Hospitals are places of healing, but they come with a hidden environmental cost. From energy-hungry buildings and single-use medical supplies to complex supply chains and anaesthetic gases, healthcare generates a surprisingly large carbon footprint. Globally, the health sector is responsible for nearly 5% of all greenhouse gas emissions, more than aviation or shipping. And yet, very few hospitals actually know the size or sources of their emissions.
NZHI’s first full sustainability report for the Maria Middelares-hospital group marks a milestone. The group manages 707 accredited beds across two hospital campuses and two polyclinics. In 2025, it became one of the world’s first healthcare institutions to measure its full CO₂ footprint across all major domains, including medical goods, staff transport, patient meals, waste, and pharmaceuticals. The result: 35,288.3 tonnes of CO₂-equivalent emissions in 2024.
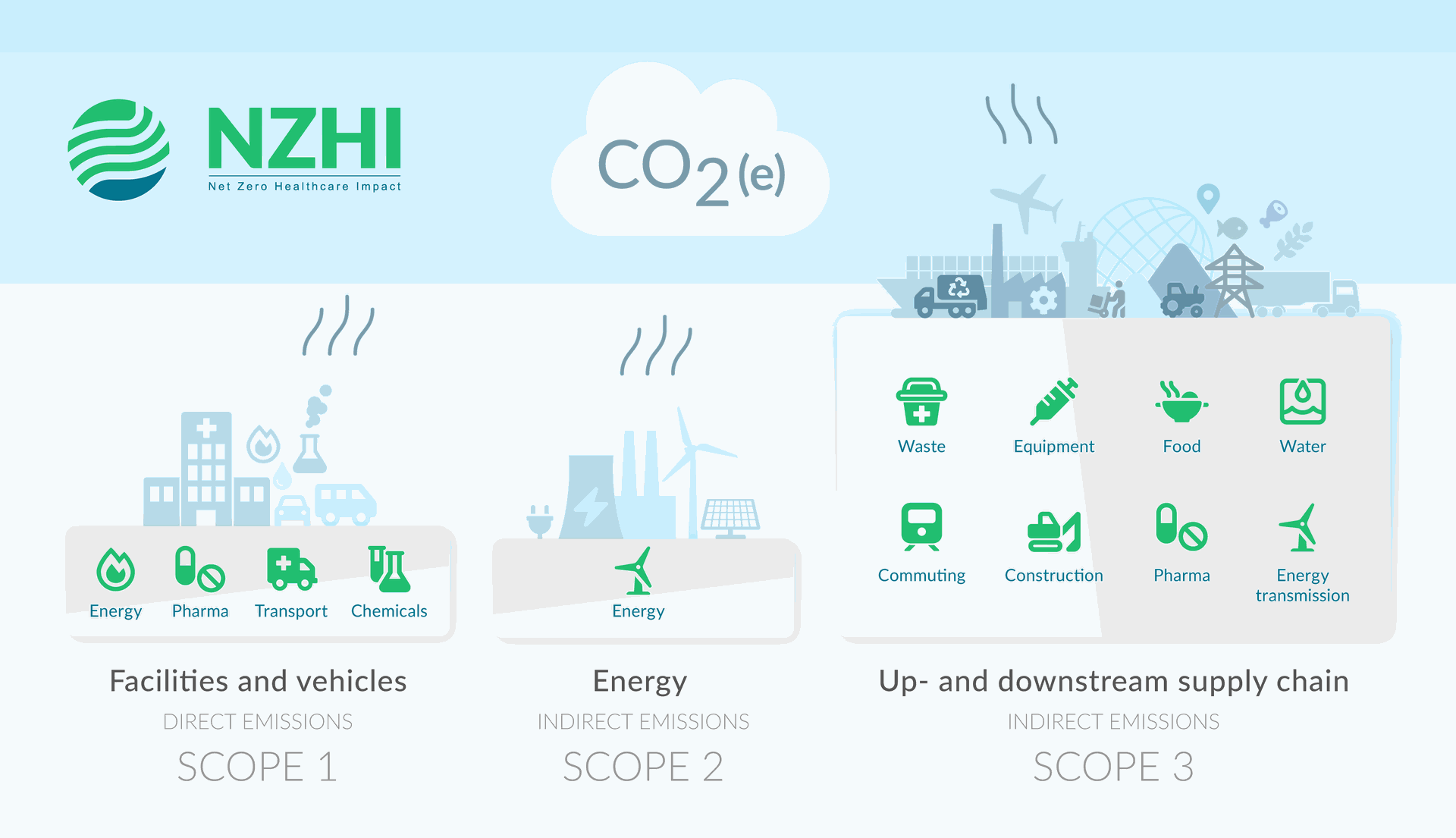
What makes this initiative stand out is not just the number, but the method behind it. The footprint was calculated according to the international Greenhouse Gas Protocol and covers all three emission scopes; from on-site heating and vehicle use (Scope 1), indirect emissions from energy use (Scope 2) to supply chain emissions and patient-related travel (Scope 3). Over 90% of the group’s climate impact turned out to come from indirect, upstream sources (Scope 3), far beyond what is traditionally monitored. Understanding this full footprint opens the door to smarter climate action. It enables hospitals to target the highest-impact areas, based on data rather than gut-feeling.
In this blog, we’ll explore how hospitals can measure their emissions, what insights this reveals, and how it can drive real change using NZHI’s first sustainability-report as a guiding example.
Measuring a Hospital’s Footprint: From Heating to Eye Injections
How do you measure the climate impact of a hospital? It’s more complex than simply checking energy bills. A comprehensive emissions analysis requires looking at the full range of hospital activities, from heating systems and surgical equipment to food services and pharmaceutical use. NZHI uses a domain-based approach, assessing emissions across 10 key areas such as energy, transport, food, pharma, medical goods, and waste. Each domain is analysed using a combination of local data, staff input, and scientifically validated life cycle assessment (LCA) sources.
The results often challenge expectations. Energy use, while highly visible, typically accounts for less than 10% of the organisation’s total carbon footprint. Much larger contributors are found elsewhere: pharmaceutical products, medical consumables (like PPE and surgical kits), and transport-related emissions. In this hospital, just a few high-impact medications drive a significant portion of pharmaceutical emissions, particularly specialized products with energy-intensive production and packaging requirements.
Anaesthetic gases are another important source of emissions. Inhalational anaesthetic agents can have a global warming potential thousands of times higher than CO₂. Mobility-related emissions, such as staff commuting and patient transport, also proved substantial.
Mobility-related emissions, such as staff commuting and patient transport, also proved substantial. While harder to measure directly, these can be estimated through mobility surveys and transport modelling, allowing hospitals to identify improvement opportunities such as active travel policies or low-emission shuttle services.
What Are the Biggest Emission Sources in Hospitals?
Hospitals are complex ecosystems, and so are their emissions. A full CO₂ footprint reveals that the climate impact of healthcare extends far beyond energy consumption. In fact, a detailed analysis showed that in this case, over 90% of emissions came from indirect sources in the broader supply chain. The footprint was broken down across ten domains, offering a clear picture of where emissions are concentrated:
- Medical goods emerged as the single largest contributor, responsible for nearly one-third of total emissions. This includes everything from surgical instruments and IV bags to disposable gowns and gloves.
- Pharmaceuticals followed closely, contributing around 29% of the footprint. Catching the eye, quite literally, just two injected eye drugs accounted for almost 28,5% of pharma-related emissions.
- Transport-related emissions made up 14%, including commuting by staff, patient travel, and business-related mobility. Based on surveys and modelling, car use was by far the dominant mode of transport.
- Food services accounted for 10% of the organisation’s total carbon footprint. Meals for patients and staff, particularly those with high meat content, were significant contributors. Data on food waste offers valuable insight into avoidable emissions.
- Building energy use (incl. heating, ventilation, and cooling) accounted for just under 10% of the total footprint, a relatively low share thanks to the organisation’s use of certified local green electricity. The report showed that energy consumption per patient admission decreased significantly, from over 350 kWh to approximately 250 kWh in 2024. Because the hospital exclusively purchases electricity from 100% green sources, it does not generate indirect greenhouse gas emissions associated with energy use (Scope 2).
- Smaller but still relevant contributors to the overall footprint included water use (<1%), construction activities (4%), and waste management (2%). Notably, waste generation per patient admission has decreased by approximately 20% since 2020. In addition, the proportion of waste classified as recyclable has improved by 25%, signalling progress in both waste reduction and sorting practices.
This domain-level analysis provides a crucial insight: the biggest climate levers in healthcare often lie outside traditional sustainability focus areas such as energy. Instead, high-impact opportunities are found in pharmaceuticals and medical goods. By shifting the focus toward these often-overlooked domains and backing it with robust data, hospitals can target the emissions that matter most, without compromising care quality.
From Insight to Impact
Building a full carbon footprint-report is only the beginning. The real value lies in what is done with the insights. Based on the detailed analysis across ten operational domains, the report presents a strategic foundation for climate action. This action is not limited to technical fixes, but extends to how care is delivered, goods are procured, and processes are organised.
The recommendations call for a shift toward circular practices in medical consumables, with clinical teams reassessing care pathways to reduce dependence on single-use items. Waste strategies should be revisited in collaboration with contractors to boost recycling and reduce incineration. In pharmaceuticals, improved stock management is encouraged to minimise expired medication, while hospitals are urged to engage suppliers of high-impact drugs to reduce emissions across their lifecycle. Mobility recommendations include supporting telemedicine and hybrid work while investing in active and electric transport. Food services are advised to transition to more plant-based, locally sourced meals and use digital tools to tackle plate waste. The report also advocates phasing out fossil gas, switching to 100% green electricity, minimising refrigerant leakage, and rethinking water use and construction through a circular lens.
The recommendations in this report were not designed to stay on paper but to serve as a foundation for action. Starting in the summer of 2025, a series of workshops were held with staff and physicians to present the findings and discuss which products and processes should be addressed first. Each session concluded with a vote on which sustainability KPIs should be prioritised, along with the proposed ambition levels for 2030. These will then be aligned with the hospital’s sustainability steering group and Green Team. Key sustainability interventions are selected and plotted as a short-, medium- or long-term action point. This participatory and data-driven approach ensures that the recommendations become part of day-to-day hospital operations and that the promised returns on investment are delivered. Going forward, the report will be updated probably bi-annually to reflect progress and identify new opportunities to reach net zero.
Why Measuring Matters
Measuring a hospital’s climate footprint is a technical task, but more importantly also a strategic enabler. Transparent reporting through dashboards, KPIs, and infographics fosters internal awareness, drives behavioural change, and engages staff across departments. It also prepares hospitals for future regulatory requirements, including the European CSRD and updated JCI sustainability standards. By proactively addressing emissions, hospitals strengthen their position in procurement processes, negotiations with suppliers and governments, and access to financing, especially as ESG performance becomes a standard expectation from funders and investors.
But perhaps the most compelling reason to measure is this: you can’t manage what you don’t monitor. Without a clear baseline, sustainability efforts risk being scattered or symbolic. A robust footprint gives hospitals the insights needed to prioritise high-impact areas, set credible targets, and track progress over time. It allows financial and operational decisions to be linked to environmental outcomes, for example through shared savings models or by factoring in CO₂ impacts in care pathway evaluations. As new frameworks like ETS2 bring a price tag to carbon, early measurement creates a head start. For a sector already experiencing the health consequences of climate change, measuring emissions isn’t just about compliance, it’s about responsibility, leadership, and preparedness.
Emission measurement is not the end goal but rather the beginning of change. By making their climate impact visible, hospitals can take targeted, evidence-based action where it matters most. Hospitals that acknowledge and monitor their emissions position themselves for greater resilience, better financial planning, and stronger credibility in a changing regulatory and climatic landscape. If one thing, this report shows that sustainability and healthcare excellence go hand in hand.
At NZHI, we help hospitals turn data into decisions and ambition into action. Whether you're starting with a footprint analysis, piloting greener processes, or developing a hospital-wide sustainability strategy, NZHI offers science-based tools, strategic guidance, and hands-on support to help you move forward. Let us help you move from intent to impact.
